Ambulance delays: ‘more paramedics’ not the solution
As an actuary who also juggles a casual role as a paramedic, Sophie Dyson has experienced the chronic issue of ambulance ‘ramping’ – the delay of paramedics handing over care of their patients to the emergency department – first-hand. While the COVID-19 pandemic has bought about innovation in healthcare delivery, ramping remains a serious issue, and a system-wide approach is needed to find a solution.
While I was working as a paramedic in Sydney last month, a man pulled up next to our parked ambulance and asked, if he went home and called Triple Zero, could an ambulance take him to a particular hospital his doctor had instructed him to go to. I wondered why he couldn’t simply continue driving to his destination. He explained he wanted to call an ambulance because parking at the hospital was difficult.
At a time when demand for ambulances is at an all-time high, this behaviour is frustrating. Ambulance ramping was a central issue to the recent Labor Party victory in South Australia, but ambulance workload and response performance is a perennial story that pre-dates the COVID-19 pandemic. Paramedics unable to respond to emergencies because they’re waiting at hospital, or callers unable to get through to Triple Zero operators because of high demand, are visible and emotive indicators that something is wrong. Increasing ambulance capacity is only a short-term fix. Ambulance services are an integral part of the health system, and a system approach is needed to find a solution.
Ramping – a system problem
Ambulance ‘ramping’ refers to paramedics being delayed in handing over care of their patients to the emergency department (ED). On arrival at ED, paramedics take patients into the ambulance bay to be triaged by the ED nurse. If there is no ED bed or treatment chair available and the patient cannot safely be transferred to the waiting room, paramedics must wait with their patient, making them unavailable to respond to other emergencies. The consequent reduction in ambulance response capacity lengthens response times.
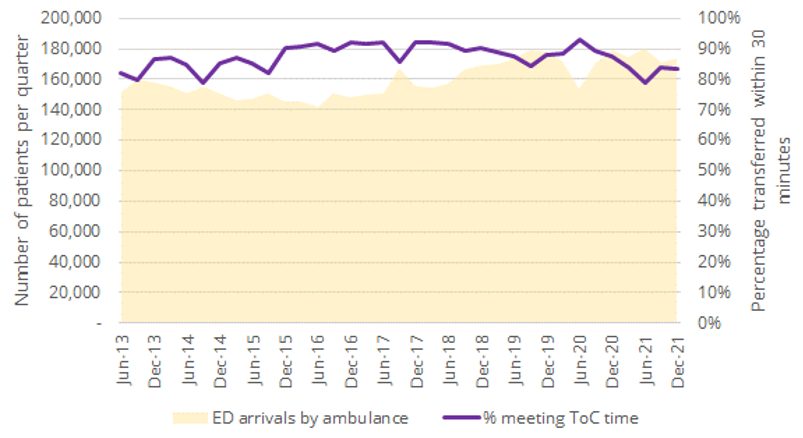
Target times for transfer of care (ToC) from paramedics to EDs vary between states. In NSW, the target is 90% within 30 minutes1, but during busy periods, ToC times can extend to several hours. As you would expect, as ED workloads rise, the proportion of patients transferred from paramedic to ED care within the target ToC time falls. The following graph shows the number of patients brought to EDs in NSW by ambulance between 2013 and 2021 compared with the proportion of patients meeting the ToC target.
Figure 1: Ambulance arrivals per quarter vs proportion of patients meeting ToC target (NSW)2
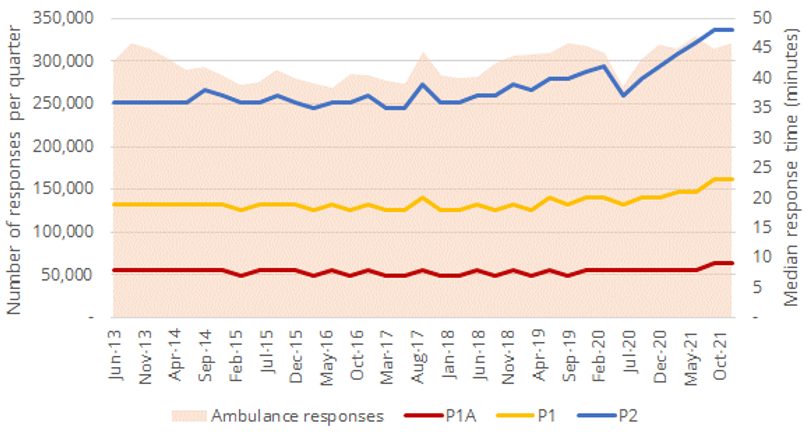
The relationship between ambulance workload and response performance is also clear. Each state determines its own response priorities; in NSW, the most urgent category is Priority 1A (P1A), all Priority 1 (P1) incidents get a lights and sirens response, and Priority 2 (P2) represents lower urgency incidents. The deterioration in response performance as ambulance workload increases is seen most dramatically in P2 median response times, as the ability to reassign vehicles to higher priority incidents has a protective effect on P1 and P1A response performance.
Figure 2: Ambulance responses per quarter vs response times by priority (NSW)3
Why is this a system problem? There are almost nine million presentations a year to Australian EDs4. Paramedics are delayed transferring patients from ambulance to ED because EDs are full, from the 25% of patients brought in by ambulance and the 75% who arrive by other means5. EDs can’t free up beds until patients are treated and discharged from ED, or transferred to a hospital ward (Australia-wide, just over 30% of ED presentations are admitted to hospital). The barrier to transferring patients from ED to wards is that the wards are full…and the barriers to discharging patients from wards include waiting for aged care or disability services, or patient transport. Downstream capacity and patient flow are the system issues here.
Financial incentives and convenience – looking behind the issue
System interrelationships exist on the demand side too, with evidence of overlapping needs in demand for ambulances, ED treatment and the 38,000 GPs providing primary care in the community. Government data6 shows that across all Australian jurisdictions, ambulance services responded to three million Triple Zero incidents in 2020-21, of which 50% did not require an emergency (lights and sirens) response and 25% of patients were able to be treated and left at home, referred to their GP or another healthcare provider. In EDs, one third of patients were deemed ‘potentially avoidable GP-type presentations’7.
Care substitution between GPs, ED and ambulance is driven by financial incentives and convenience. For example, although ambulance services are not funded by Medicare, for most patients – those with pension cards, private health insurance or an ambulance membership – ambulance care is free at the point of care and there are no financial consequences for calling Triple Zero. The cost, almost $1,100 per incident8, falls largely on state governments. For low acuity incidents, that’s a lot to pay for reassurance and a couple of paracetamol. If patients make their own way to ED for a health issue that does not result in admission, the average cost of an ED presentation nationwide, funded by Australian and State Government is $6169.
Ambulance services recognise the issue of ambulance/ED/primary care substitution and the market failure that this represents. Several services have developed initiatives to address the high cost of dispatching an ambulance to low acuity calls while at the same time providing more clinically-appropriate care – these initiatives include virtual care programs that provide telephone advice and referrals to other providers. The cost of providing virtual care, even with an ultimate referral to a private medical provider, is less than half that of sending an ambulance. Heightened demand during COVID-19 has resulted in an expansion of these services. From an ambulance perspective, they demonstrate an entirely rational response. However, from a whole-of-system perspective, the cost to Government is still several multiples of what would be paid via Medicare for a telehealth consultation with a GP10.
Where can we look for a solution?
The pandemic has been a time of innovation in healthcare delivery. Telehealth, originally introduced to support service provision in rural areas, has become the default method for talking to our family doctor. Smartphone apps record COVID-19 patients’ vital signs and detect early indicators of deterioration. Algorithms predict the COVID-19 patients most at risk of hospitalisation and target patient monitoring resources more effectively.
With light at the end of the COVID-19 tunnel, we need to sustain the spirit of innovation and action to develop longer-term solutions to extended ambulance ToC and response times (and other health-system problems while we’re at it). To do this, both demand and supply issues need to be tackled, as well as improving patient flow and care coordination. Australia’s health system delivers an enviable level of care, but overlapping state and Commonwealth responsibilities have always created opportunities for blame- and cost-shifting11. The rapid introduction of certain COVID-19 initiatives has exacerbated this situation, with similar services accessible through different pathways and a blurring of health-service responsibilities.
Navigating the path towards a comprehensive approach
When developing future solutions, we need to remove duplication and substitution, consider solutions through a whole-of-system lens rather than from the perspective of a single provider, and recognise the financial and other incentives that drive healthcare demand and supply.
Back to the driver who wanted to call Triple Zero to overcome the inconvenience of parking. Consider the financial impact of lost revenue if hospital parking for ED attendances was subsidised, compared with the savings from reducing the unnecessary dispatch of ambulances. How could these savings be applied to expand service delivery and provide more appropriate clinical care?
Next time ambulance ramping is in the news, don’t think ‘we need more paramedics’ (though that’s always a welcome thought), think ‘we need to capitalise on COVID-19 ingenuity, develop sustainable solutions addressing both demand and supply, and take a whole-of-system view that recognises financial and other incentives’. Even though it doesn’t make a catchy soundbite.
|
References
|
CPD: Actuaries Institute Members can claim two CPD points for every hour of reading articles on Actuaries Digital.