COVID-19: Excess mortality for May 2022 at similarly high levels to earlier in 2022
Catch up on the Actuaries Institute’s COVID-19 Mortality Working Group’s latest analysis of excess deaths.
In summary:
|
![]()
Background
The COVID-19 Mortality Working Group has examined the latest Provisional Mortality Statistics, covering deaths that occurred prior to 31 May 2022 and were registered by 31 July 2022, released by the Australian Bureau of Statistics (ABS) on 26 August. This release also includes the article COVID-19 Mortality in Australia which includes details on all COVID-19 deaths that occurred and were registered by 31 July 2022.
We have compared the observed deaths to our ‘baseline’ predicted number of deaths for doctor-certified deaths (by cause) and coroner-referred deaths (for all causes combined).
We have also provided an indicative estimate of excess mortality due to COVID-19 only, for the three months subsequent to the ABS data (June to August 2022).
Baseline prediction
Our previous Actuaries Digital article discussed in some detail how we have arrived at our baseline predicted deaths. In short, our baselines are set by extrapolating linear regression models fitted to standardised death rates (SDRs), which are then re-expressed as numbers of deaths. For the pandemic years, we have included different years to train the regression models:
- For 2020 and 2021, we have used the 2015-19 experience.
- For 2022, we have:
- used 2015-19 experience to set our baseline for deaths from respiratory disease and dementia, on the basis that 2020 and 2021 experience for these causes was materially affected by the pandemic;
- also shown the average experience in 2020-21, for reference, when analysing mortality from these causes; and
- used 2015-21 experience to set our baseline for deaths from all other causes and for coroner-referred deaths, on the basis that it is likely that 2020 and 2021 experience more closely reflects a slow-down in underlying mortality improvement than the impacts of the pandemic.
- used 2015-19 experience to set our baseline for deaths from respiratory disease and dementia, on the basis that 2020 and 2021 experience for these causes was materially affected by the pandemic;
Our estimates of excess deaths remain ‘in the absence of the pandemic’ for each of the three years 2020 to 2022. We have not included any COVID-19 deaths in the baseline, as these would not exist in the absence of the pandemic.
As always, it is important to note that predicted death numbers are increasing faster from demographic changes (ageing and population size) than they are reducing due to mortality improvement. Therefore, our model predicts higher baseline numbers of deaths in each successive year.
![]()
Excess deaths to 31 May 2022
Figure 1 and Table 1 below summarise the results of our analysis. This article concentrates on the experience in 2022, but we have also shown the 2020 and 2021 results for context.
Table 1 differs a little from previous articles in that we have formed an estimate of the share of coroner-referred deaths that were from COVID-19 (previously we have only shown doctor-certified COVID-19 deaths). Our estimate of coroner-referred COVID-19 deaths is discussed in a later section.
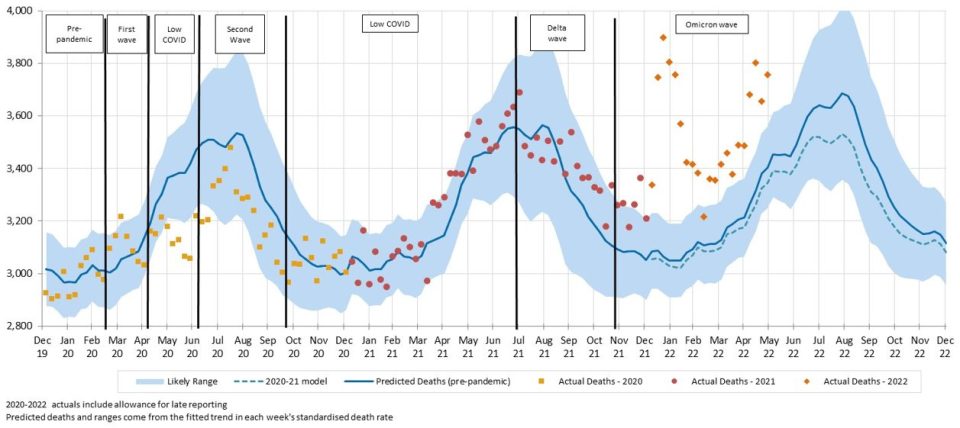
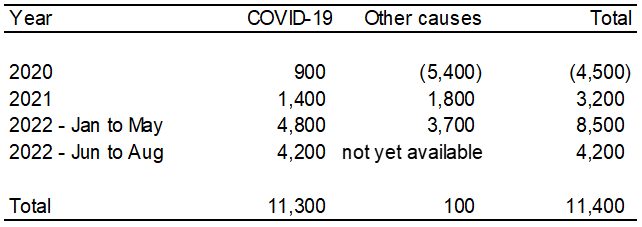
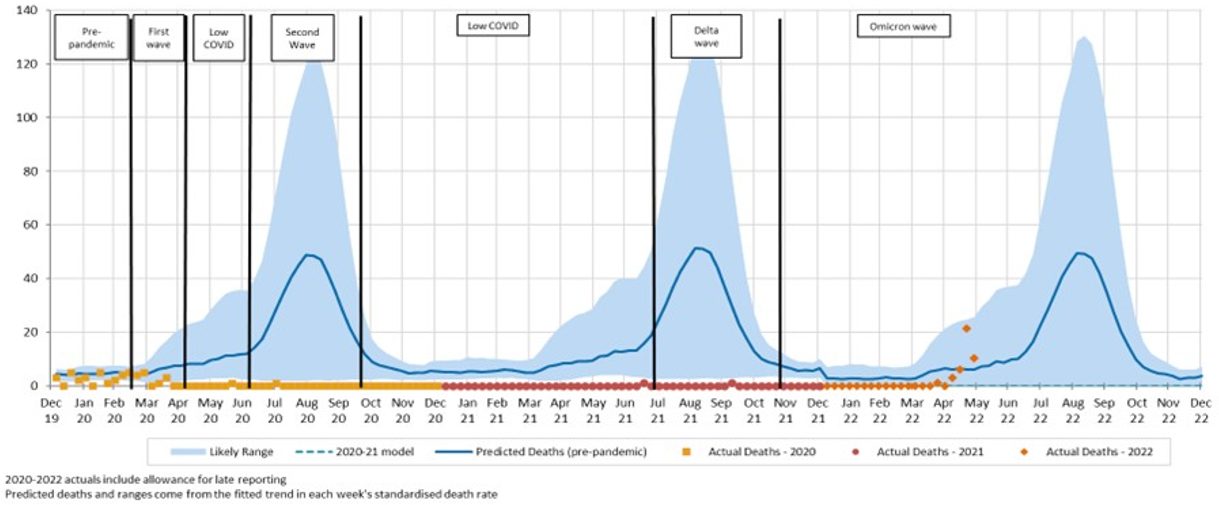
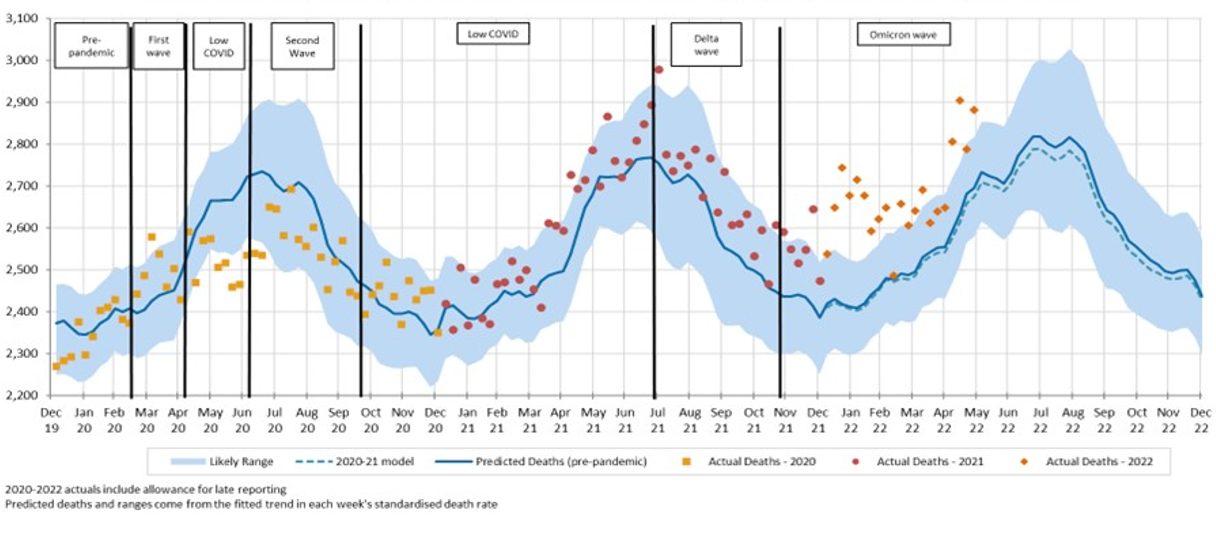
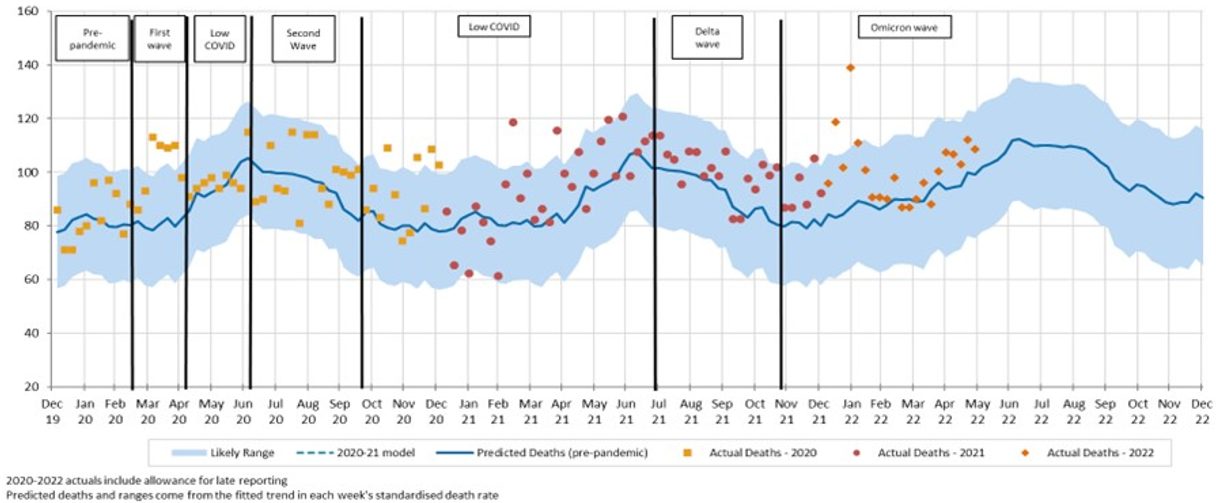
Figure 1 – Weekly actual and predicted deaths in Australia – All causes
Deaths in the most recent four weeks were again well above the upper end of the prediction interval (i.e. above the 97.5th percentile). So far, all but one week of 2022 has been above the 97.5th percentile.
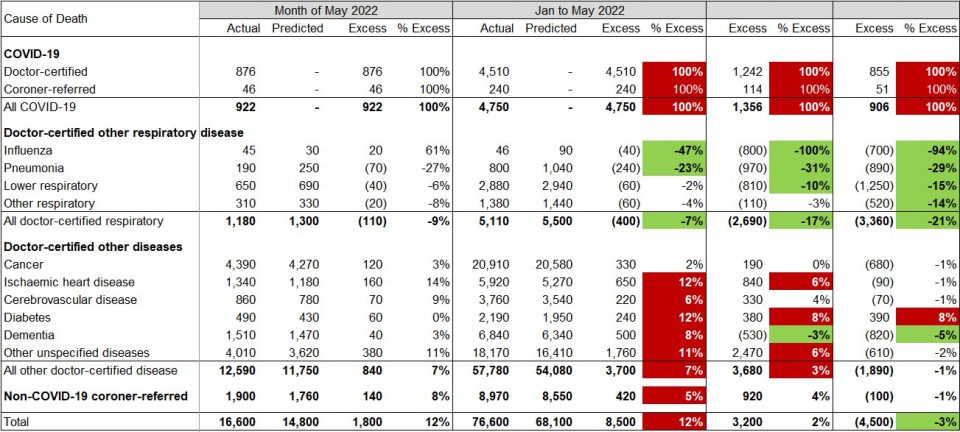
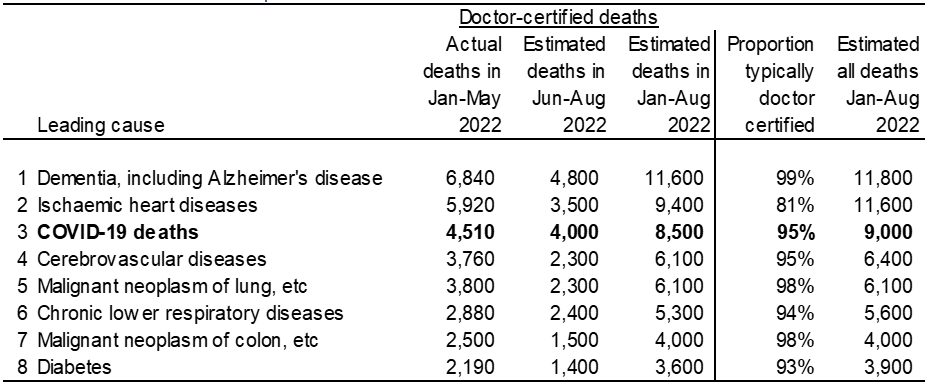
Table 1 – Excess deaths in Australia
*Figures shaded green indicate that the observed values are below the 95% prediction interval while figures shaded red are above the 95% prediction interval
For the month of May 2022, total deaths were 12% (or +1,800) higher than predicted. Around half of the excess deaths were due to COVID-19. Both ischaemic heart disease and other unspecified causes also made a significant contribution to excess deaths. Cancer deaths were up a little, the result of one high outlier week rather than an overall higher trend for the month.
For the first five months of 2022, total deaths were 12% (or +8,500) higher than predicted. This compares with excess deaths of -4,500 for 2020 and +3,200 for 2021.
By cause, in aggregate for these five months:
- there were 4,750 deaths from COVID-19, representing just over 50% of the excess deaths. 77 of these deaths were reported as due to Long COVID;
- doctor-certified deaths from respiratory disease continued to be lower than expected (down 7% or 400), despite May having the first sizeable number of influenza deaths since April 2020;
- doctor-certified deaths from cancer were close to expected, as has been the case so far throughout the pandemic;
- doctor-certified deaths from heart disease, cerebrovascular disease, diabetes and dementia were all higher than predicted (by between 6% and 12%, or a total of 1,610);
- doctor-certified deaths from other unspecified diseases were higher than predicted (by 11% or 1,760), continuing a trend observed since April 2021. Note that this is a large ‘catch-all’ category and it is difficult to infer the reason for this large increase, although history suggests that non-ischaemic heart diseases probably make up around 25% of deaths from other unspecified causes; and
- non-COVID-19 coroner-referred deaths were 5% (+420) higher than expected.
Data included in the article COVID-19 Mortality in Australia shows that, in the first five months of 2022, there were 999 deaths in people who were COVID-19 positive at death but where COVID-19 was not the primary cause of death. This means that COVID-19 was a potential contributory factor in around one-quarter of the excess mortality from non-COVID-19 causes.
![]()
Coroner-referred COVID-19 deaths
The Provisional Mortality Statistics includes the number of deaths from COVID-19 that were doctor-certified, while the COVID-19 Mortality in Australia article includes total deaths from COVID-19. Taking the difference between the two gives the number of coroner-certified COVID-19 deaths.
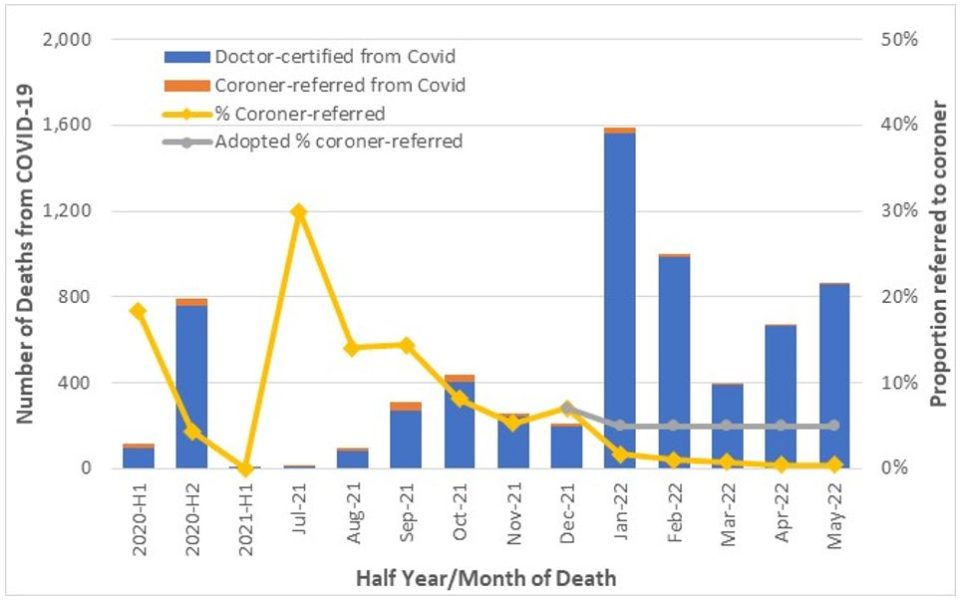
Figure 2 shows the number of deaths from COVID-19 split between doctor-certified and coroner-referred, plus the proportion that are coroner-referred.
Figure 2– Doctor-certified versus Coroner-referred COVID-19 deaths
In 2020 and early 2021, Australia experienced relatively small numbers of COVID-19 deaths and the proportion that were coroner-referred varied quite significantly given the low numbers. We have assumed that coroner-referred COVID-19 deaths will be 5% of all COVID-19 deaths in 2022, based on the experience of late 2021. We have deducted these estimated coroner-referred COVID-19 deaths from other coroner-referred deaths.
If our estimate of coroner-referred COVID-19 deaths is too high (or low), this will not affect the total level of excess deaths measured. It will just mean that our estimate of non-COVID-19 coroner-referred deaths will be too low (or high) by the same amount.
![]()
Comparison with ABS reporting
The results that we present here differ from those quoted by the ABS in its commentary surrounding the release of the Provisional Mortality Statistics.
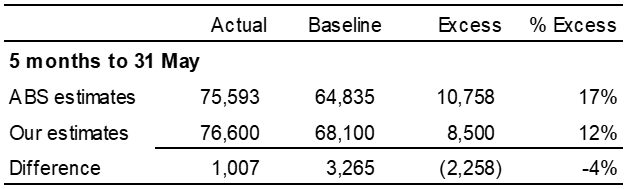
Table 2 – Comparison with ABS Figures for 2022
The ABS has reported about 10,800 (17%) excess deaths in the first five months of 2022, in comparison with our estimate of 8,500 (12%).
We have made allowance in our estimate for late registered deaths whereas the ABS does not. This acts to understate the ‘actual’ number of deaths used by the ABS, thus understating the measure of excess deaths by around 2%.
However, the more significant difference is in the determination of the baseline, where the ABS uses a simple average of the number of deaths from 2017, 2018, 2019 and 2021, with no allowance for mortality trends or demographic changes. In our view, this understates the baseline and therefore overstates the measure of excess deaths by around 6%.
These two impacts work in opposing directions, resulting in a difference in the estimates of excess deaths of around 4%.
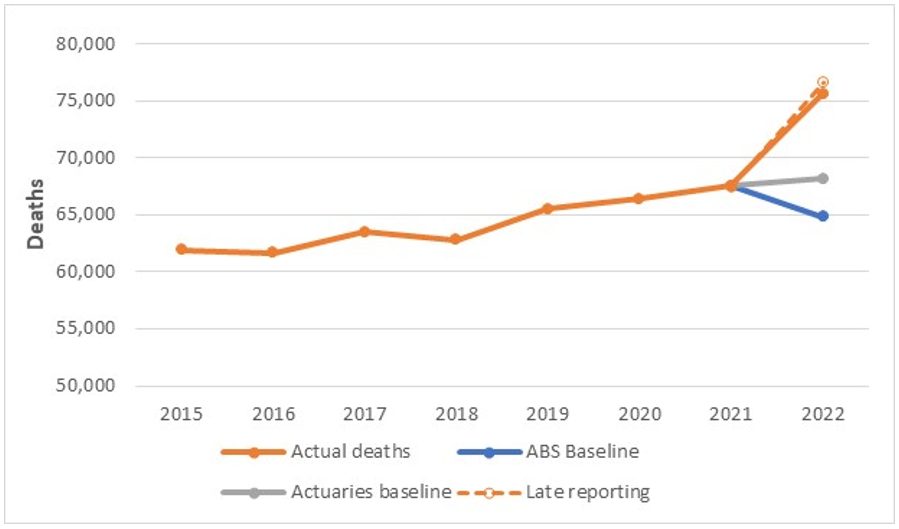
Figure 3 shows the trend in actual deaths in the first five months of each year, along with the ABS baseline, our baseline and our allowance for late registered deaths.
Figure 3 – Deaths in five months to 31 May of each year
The graph demonstrates how significant the jump in January to May mortality has been in 2022, compared with the trend of previous years. It also shows that the ABS baseline is surely too low.
![]()
COVID-19 deaths in June to August 2022
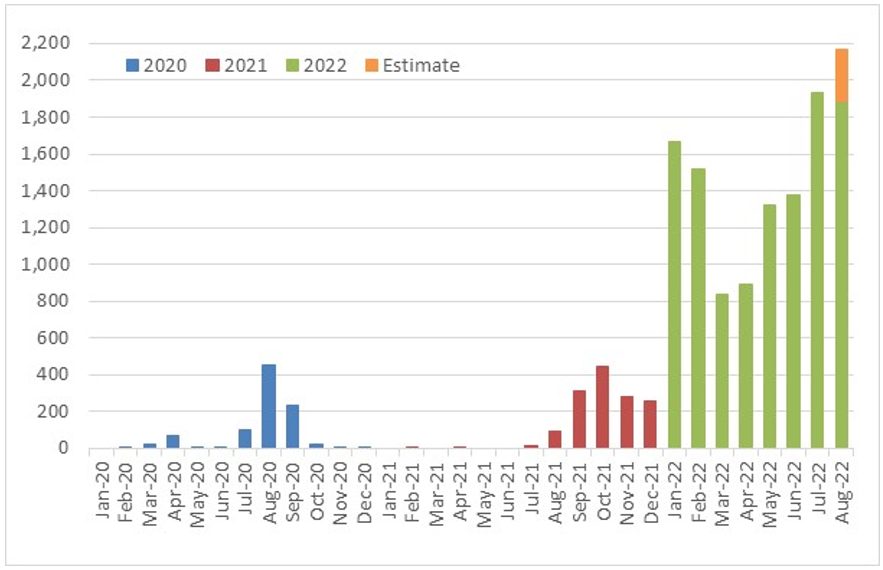
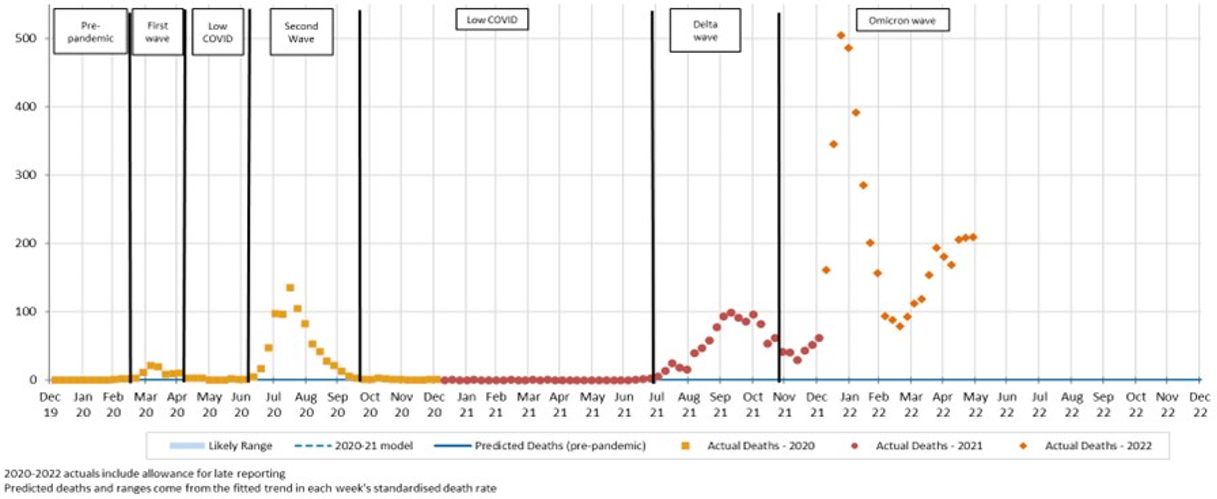
While the ABS provisional mortality statistics data is only available until the end of May 2022, surveillance COVID-19 deaths are available daily. Figure 4 shows the number of such deaths in each month of 2020, 2021 and the first eight months of 2022 (noting that the month of August includes actual data to 28 August plus an estimate for the remaining three days of the month).
Figure 4 – COVID-19 deaths in Australia, reported from surveillance systems*
* On 31 March, NSW Health released a report that detailed the outcomes of a reconciliation between their daily death counts and data held by Births, Deaths and Marriages (which is the basis of the ABS data). This reconciliation identified 331 deaths that had not been captured in the daily counts. We have allocated these deaths to the months when the deaths occurred.
There were 912 surveillance COVID-19 deaths in 2020 and a further 1,402 deaths in 2021. In the eight months to 31 August 2022, there have been 11,720 COVID-19 deaths. Of these, 5,480 occurred in the three months to 31 August 2022 (where we have no provisional mortality statistics for all causes). Following a record July, surveillance deaths in the month of August 2022 are the highest yet recorded.
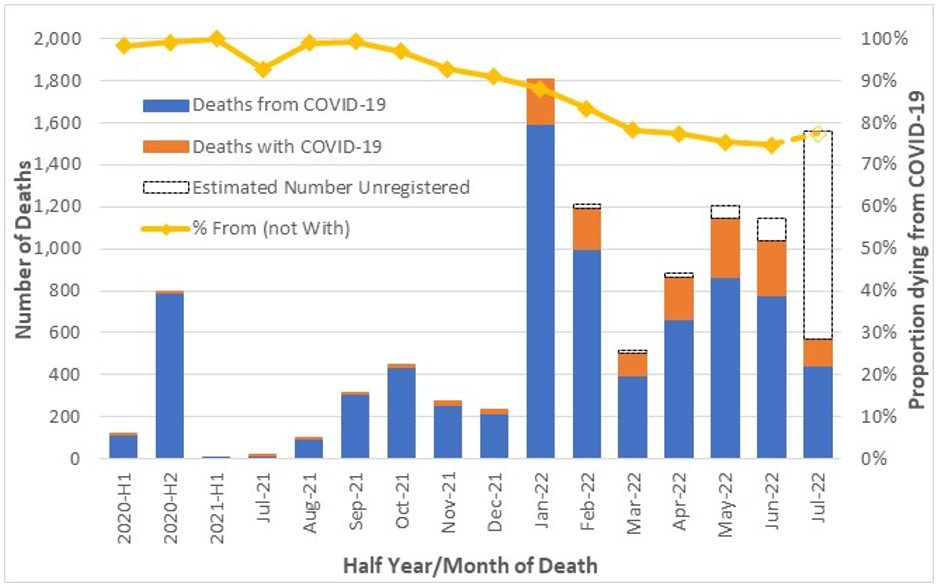
The COVID-19 Mortality in Australia article shows that, since the Omicron wave, COVID-19 was the underlying cause of death on a reducing proportion of death certificates mentioning COVID-19. Figure 5 shows a comparison of deaths ‘from’ COVID-19 versus those ‘with’ COVID-19, noting that, for the most recent months, a large proportion of deaths have not yet been registered (the estimated numbers of unregistered deaths are also shown). Figure 5 also contains a line showing the proportion of registered COVID-19-related deaths that were ‘from’ rather than ‘with’ COVID-19.
Figure 5 – A comparison of deaths ‘from’ COVID-19 to those ‘with’ COVID-19 (source: ABS)
The proportion of registered COVID-19 deaths from COVID-19 has reduced in 2022, from 88% in January to between 75% and 77% in March to July. A large number of deaths are still to be registered in July, so this percentage could change – hence, this point is shown as a preliminary estimate.
We consider it reasonable to assume that, of the 5,480 COVID-19 deaths reported from June to August 2022, around 76% may have been from COVID-19 rather than with COVID-19. Therefore, we estimate that around 4,200 deaths in this period may have been due to COVID-19.
Our prediction model suggests that, without a pandemic, there would have been a total of around 46,900 deaths in the three months from June to August 2022.
Thus, COVID-19 deaths represent around 9% extra mortality from June to August 2022 (around 7% in June, 9% in July and 10% in August). There have probably been fewer deaths from respiratory diseases in this period than our pre-pandemic predictions. However, we consider it likely that mortality from non-COVID-19, non-respiratory causes will be higher than our pre-pandemic predictions, given the higher-than-expected mortality in 2021 and early 2022, and that this will outweigh the benefit from respiratory disease. Therefore, we expect that total excess mortality from June to August 2022 will have been higher than the 9% explained by COVID-19.
Excess mortality across the pandemic
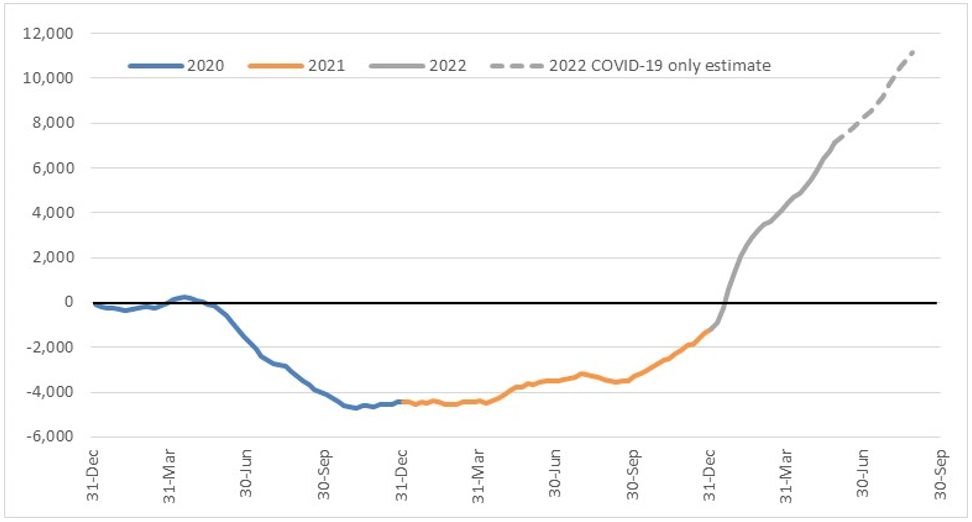
Figure 6 combines our preliminary estimate of excess deaths due to COVID-19 only for June to August 2022 with our detailed excess death estimates shown earlier, to reveal cumulative excess mortality since the start of 2020.
Figure 6 – Estimated cumulative excess deaths in Australia since 1 January 2020
Deaths from the Delta wave in the latter part of 2021 and the Omicron wave in early 2022 had fully eroded the negative excess deaths experienced earlier in the pandemic by early January 2022. Cumulatively across the pandemic, our conservative estimate is that Australia had experienced around 11,400 excess deaths by the end of August 2022. This represents an average excess mortality rate of about 2.5% over that time.
These impacts by year can be seen separated into excess deaths from COVID-19 and other causes in the table below.
Table 3 – Excess deaths separated into COVID-19 and other causes
We estimate that there have been 11,300 deaths from COVID-19 in Australia to the end of August 2022.
For non-COVID-19 causes, lower than predicted deaths in 2020 have been fully offset by higher than predicted deaths in 2021 and the five months to 31 May 2022.
What could be causing the non-COVID-19 excess deaths?
The measurement of higher numbers of deaths than predicted does not tell us why this is occurring. There are a number of reasons hypothesised around the world (where this effect is occurring to a greater or lesser extent), including:
1. Post-COVID-19 sequelae or interactions with other causes of death:
An earlier COVID-19 illness could be causing later illness and death, and/or COVID-19 could have worsened other diseases which ultimately caused death. Studies have shown that COVID-19 is associated with higher subsequent mortality risk from heart disease and other causes. To some extent, this shows on death certificates in the 999 deaths in the first four months of 2022 where COVID-19 is listed as a contributory cause, and a further 77 deaths were identified as from Long COVID. However, we understand that medical science has not yet established a causative link that would allow, say, a heart attack several months after a COVID-19 infection to be attributed back to COVID-19. As such, it seems likely that there would be more of these deaths than identified.
Possible impact in Australia: High
2. Delayed deaths from other causes:
Some of the reduction in deaths in 2020 and 2021 that resulted from the absence of many respiratory diseases may be reversing. People who otherwise may have died of flu or other respiratory diseases in those years had their systems been stressed may now be succumbing to their underlying illnesses.
Possible impact in Australia: Moderate
3. Delay in emergency care:
Pressure on the health, hospital and aged care systems, including ambulance ramping and bed block, could lead to people not getting the care they require, either as they avoid seeking help, or their care is not as timely as it might have been in pre-pandemic times.
Possible impact in Australia: Low to Moderate
4. Delay in routine care:
Lack of earlier diagnostic testing for non-COVID-19 causes and delays in elective surgery could lead to later mortality. While this does not yet appear to be occurring for cancer deaths, it may be a factor in higher deaths from other causes, such as ischaemic heart disease, diabetes, and the large ‘other’ category.
Possible impact in Australia: Low to Moderate
5. Pandemic-influenced lifestyle changes:
There is evidence from the UK that a higher proportion of people made less healthy lifestyle choices during lockdowns (e.g. drinking more alcohol, exercising less, higher rates of childhood obesity), and that these less healthy practices have continued. It is unclear to what extent similar factors may be affecting mortality in Australia in 2022. Deaths directly caused by drug and/or alcohol abuse are relatively low, compared with those from other causes, but there would be an indirect impact.
Possible impact in Australia: Low
6. Vaccine-related deaths:
While there have been deaths in Australia caused by the administration of COVID-19 vaccines, the number of such deaths has been small. Australia has a very good vaccine approval and safety monitoring processes, administered by the Therapeutic Goods Administration. The latest vaccine safety report (to 25 August) shows 136,000 adverse events have been reported from 63 million vaccines administered (a rate of 0.2% per vaccine administered). Of those adverse events, 931 were reports of death following vaccination. Of those deaths, 13 were found to have been caused by the administration of the vaccine, and all were following a first dose of AstraZeneca which is now in limited use in Australia.
Possible impact in Australia: Negligible
7. Undiagnosed COVID-19:
Some of the excess deaths could actually be from non-identified COVID-19. This effect happened early in the pandemic, but seems less likely in 2022, as testing is much more available, particularly for those who are seriously ill. Also, for any deaths where COVID-19 may be suspected, post-mortem testing is occurring in Australia.
Possible impact in Australia: Negligible
It is not possible to identify from death counts alone whether any or all of these issues are causing the non-COVID-19 excess deaths, but we think that they are the most likely explanations.
![]()
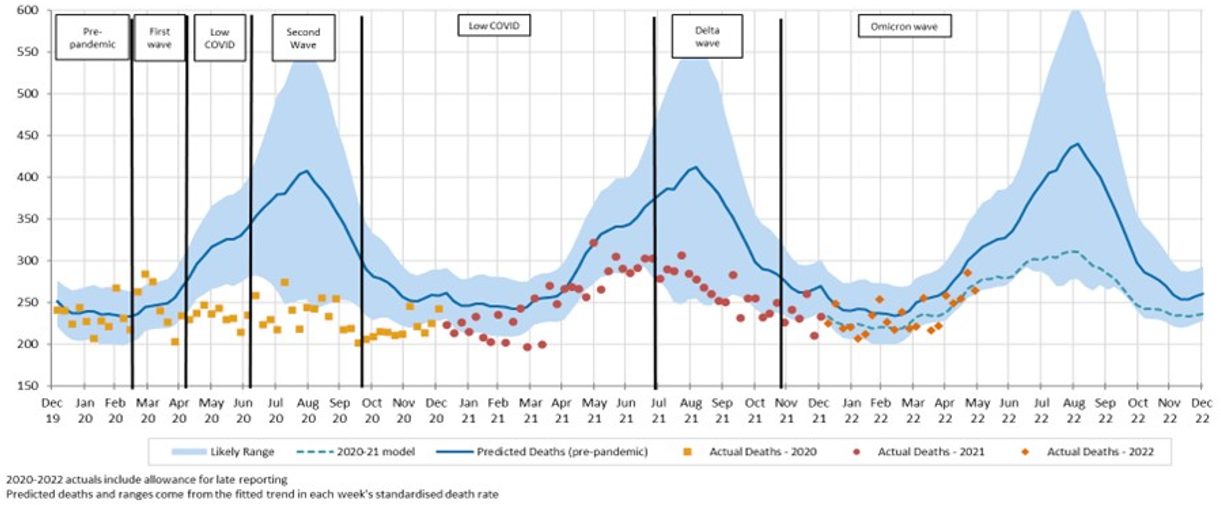
Leading causes of death
In this section, we assess where COVID-19 sits in terms of leading causes of death in Australia.
By way of background, each death in Australia is coded with a primary cause of death based on the International Classification of Diseases, version 10 (ICD-10). The ICD-10 classification system is hierarchical, so depending on how you add up the classifications, the leading causes of death may differ. Cancer, for example, is the cause of death in about 50,000 deaths per annum putting ‘all cancers’ clearly as the leading cause of death. However, the individual cancer that causes the highest number of deaths is lung cancer at about 8,500 per annum, making it the fourth leading cause excluding COVID-19.
The ABS reports on the top 20 leading causes of death by grouping individual ICD-10 codes. Cancers are grouped based on the region of the body. In this analysis, we have followed the same classification system.
So where does COVID-19 fit? At best, we can only make an estimate as:
- the detailed cause of death data is not yet available for deaths in 2020, 2021 or 2022 (data is available for deaths registered in 2020, but data for deaths occurring in 2020 is incomplete); and
- the deaths by non-COVID-19 cause shown in Table 1 above are for doctor-certified deaths only, and cancer deaths are not available broken down by type of cancer.
We have estimated deaths for the leading causes for the first eight months of 2022. To do this, we have:
- taken doctor-certified deaths by cause to 31 May as shown in Table 1;
- added our predicted doctor-certified deaths for the three months of June to August 2022; and
- included an allowance for coroner-referred deaths (using the historical ratio of doctor-certified to coroner-referred deaths).
For the leading cancer causes, we have adopted a top-down approach. We have followed the same approach as above for cancer deaths as a whole. We have then estimated the leading cancers by using the same breakdown of cancer deaths by body part as the average for 2015-2020. Lung cancers make up around 18% of all cancer deaths while colon cancers make up around 12% of all cancer deaths. These proportions have been stable over the recent time period examined.
Table 4 – Estimated leading causes of death in the first eight months of 2022
Ischaemic heart disease has been the leading cause of death in Australia for many years. However, the mortality rate for this cause has been declining at the same time as the population has been aging, resulting in an increasing number of dementia deaths. Our estimates of the number of deaths in the first eight months of 2022 from dementia (11,800) are expected to just pass deaths from ischaemic heart disease (11,600), resulting in our expectation that dementia will be the leading cause of death in 2022.
Turning to COVID-19 deaths, we estimate deaths from COVID-19 in the first eight months of 2022 at about 9,000:
- 4,510 doctor-certified deaths in five months to May; plus
- 240 coroner-referred deaths in the five months to May; plus
- 4,200 deaths in the three months from June to August (of which an estimated 4,000 are doctor-certified and 200 coroner-referred).
This would put COVID-19 as the third leading cause of death for the first eight months of 2022, well behind dementia and ischaemic heart diseases with around 11,600-11,800 deaths each, but materially higher than cerebrovascular diseases (largely stroke) at around 6,400 and cancers of the lung at 6,100.
|
The remainder of this article shows actual versus predicted deaths to 31 May 2022. Analysis and discussion of individual causes of death refer to doctor-certified deaths, while coroner-referred deaths are shown for all causes combined (including COVID-19).
|
COVID-19 deaths
Figure 7 – Weekly actual and predicted doctor-certified deaths in Australia – COVID-19
There were 876 doctor-certified deaths from COVID-19 in May 2022, compared with 1,325 surveillance deaths (449 fewer). We would not expect the numbers to be identical, because:
- there are delays between time of death and lodgement of the doctor’s certificate;
- the reporting criteria are different, with the main difference being that the surveillance reporting includes all deaths in people who have died while COVID-19 positive and without another clearly obvious unrelated cause (e.g. trauma), whereas the ABS deaths included in this chart only include deaths where COVID-19 was certified as the primary cause of death; and
- some COVID-19 deaths will be referred to the coroner (e.g. deaths occurring at home).
COVID-19 deaths in 2022 have far exceeded deaths from this cause earlier in the pandemic and COVID-19 deaths in May 2022 were higher than in both March and April.
![]()
Deaths from Respiratory Disease
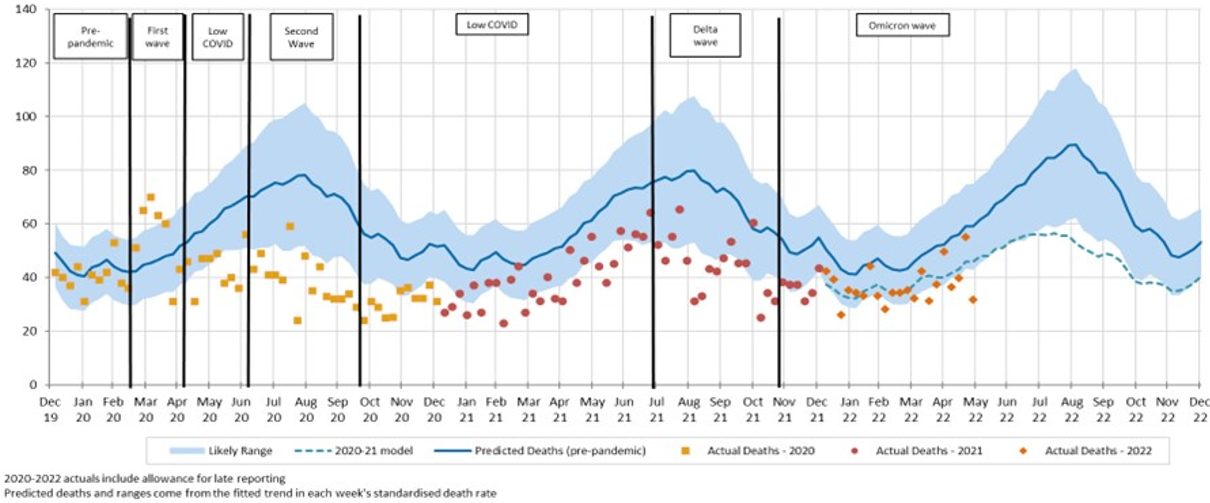
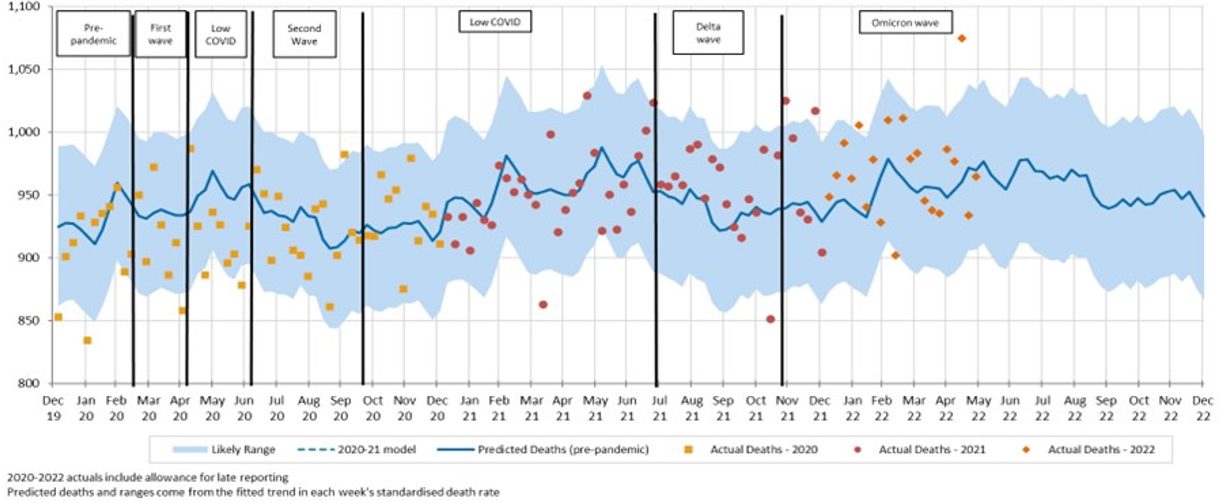
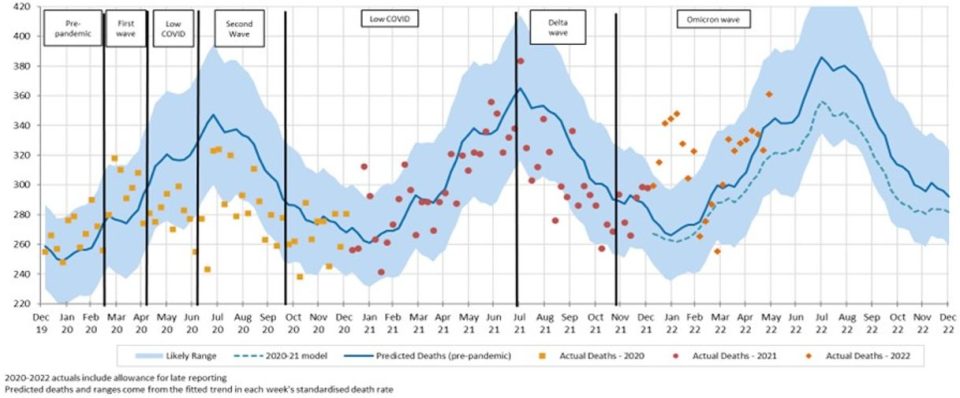
Figure 8 – Weekly actual and predicted doctor-certified deaths in Australia – all respiratory diseases
In the five weeks of May 2022, deaths from respiratory disease were close to or lower than predicted, following the trend throughout most of the pandemic.
The following figures present a breakdown of respiratory disease into influenza, pneumonia, lower respiratory disease, and other respiratory disease.
Figure 9 – Weekly actual and predicted doctor-certified deaths in Australia – Influenza
There were 45 influenza deaths in the month of May, the first time that there has been more than 1 influenza death in a month since April 2020.
Figure 10 – Weekly actual and predicted doctor-certified deaths in Australia – Pneumonia
There were fewer deaths from pneumonia in May 2022 than predicted, and they were below the bottom end of the 95% prediction interval in three of the five weeks. Deaths so far in 2022 are similar to the levels seen in 2020 and 2021.
Figure 11 – Weekly actual and predicted doctor-certified deaths in Australia – Lower respiratory diseases
Deaths from lower respiratory disease in May 2022 have broadly been close to predicted.
Figure 12 – Weekly actual and predicted doctor-certified deaths in Australia – Other respiratory diseases
Deaths from other respiratory diseases continue to be close to our predictions in May 2022.
![]()
Non-COVID-19 and Non-Respiratory Deaths
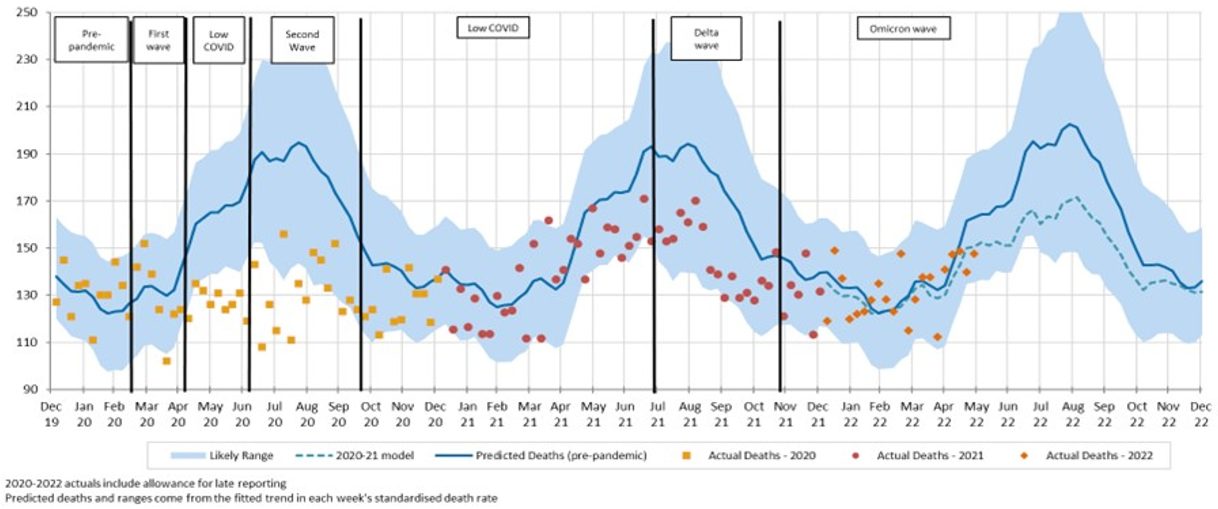
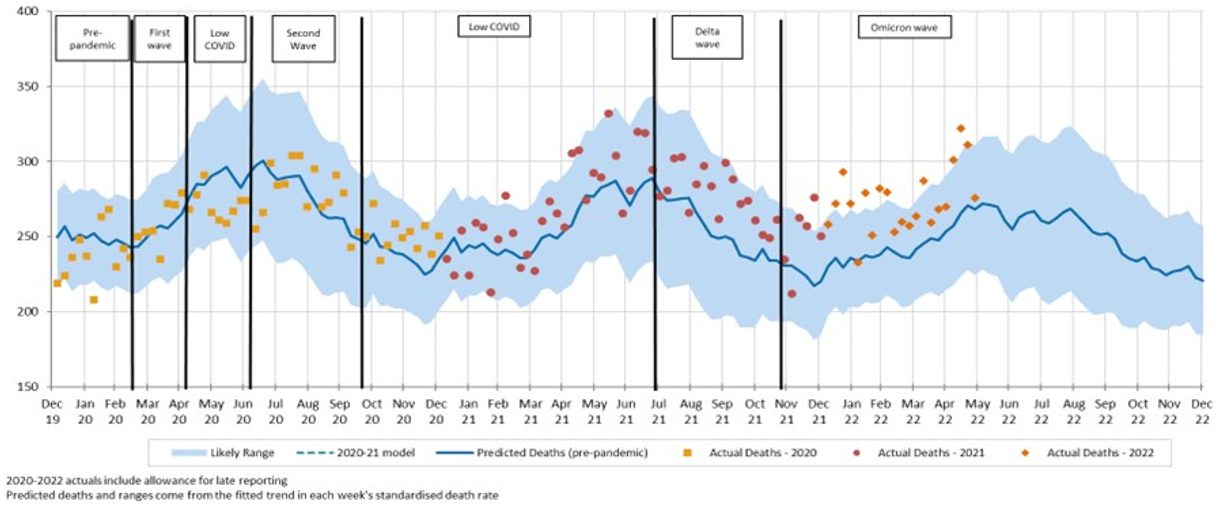
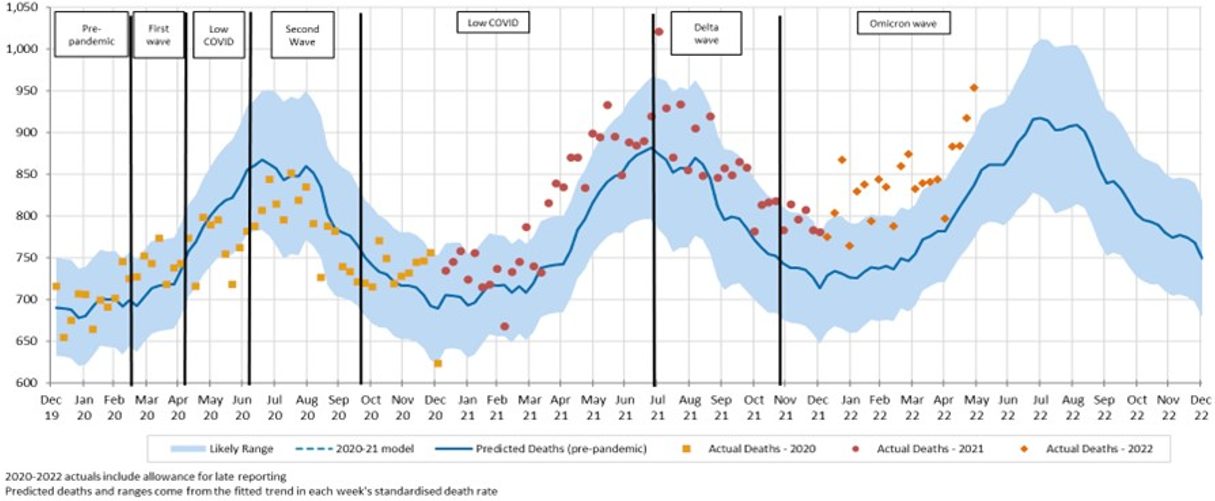
Figure 13 – Weekly actual and predicted doctor-certified deaths in Australia – All causes other than respiratory diseases and COVID-19
Excluding deaths from COVID-19 and respiratory diseases, deaths were higher than expected for all weeks in May 2022, and above the prediction interval in four of the five weeks. This is mainly driven by deaths from ischaemic heart disease, cerebrovascular disease and ‘other’ causes.
The following figures show a breakdown of non-respiratory/non-COVID-19 deaths into cancer, heart disease, cerebrovascular disease, diabetes, dementia, and all other causes.
Figure 14 – Weekly actual and predicted doctor-certified deaths in Australia – Cancer
Cancer deaths continue to be close to predicted numbers for most weeks, except for significantly more deaths in third week of May. With diagnostic testing down in 2020, there were concerns that there would be a spike in cancer deaths in 2021 and beyond. We are not yet seeing any clear evidence of this effect.
Figure 15 – Weekly actual and predicted doctor-certified deaths in Australia – Ischaemic heart disease
Deaths from ischaemic heart disease were significantly higher than predicted in the second, third, and fourth week of May, and outside the prediction interval for these weeks. Very few weeks have been below the predicted line since March 2021.
Figure 16 – Weekly actual and predicted doctor-certified deaths in Australia – Cerebrovascular disease
For cerebrovascular disease, deaths were higher than predicted for four out of the five weeks in May 2022, and above the prediction interval for two of those weeks.
Figure 17 – Weekly actual and predicted doctor-certified deaths in Australia – Diabetes
Deaths from diabetes were also higher than predicted in May 2022 although within the prediction interval.
Figure 18 – Weekly actual and predicted doctor-certified deaths in Australia – Dementia
Deaths from dementia were higher than predicted in May 2022 but were within the prediction interval.
Figure 19 – Weekly actual and predicted doctor-certified deaths in Australia – Other unspecified diseases
Deaths from other causes, i.e. those not explicitly reported on by the ABS, were again much higher than predicted in May 2022. All except one week were at or above the upper limit of the prediction interval.
![]()
Coroner-referred deaths
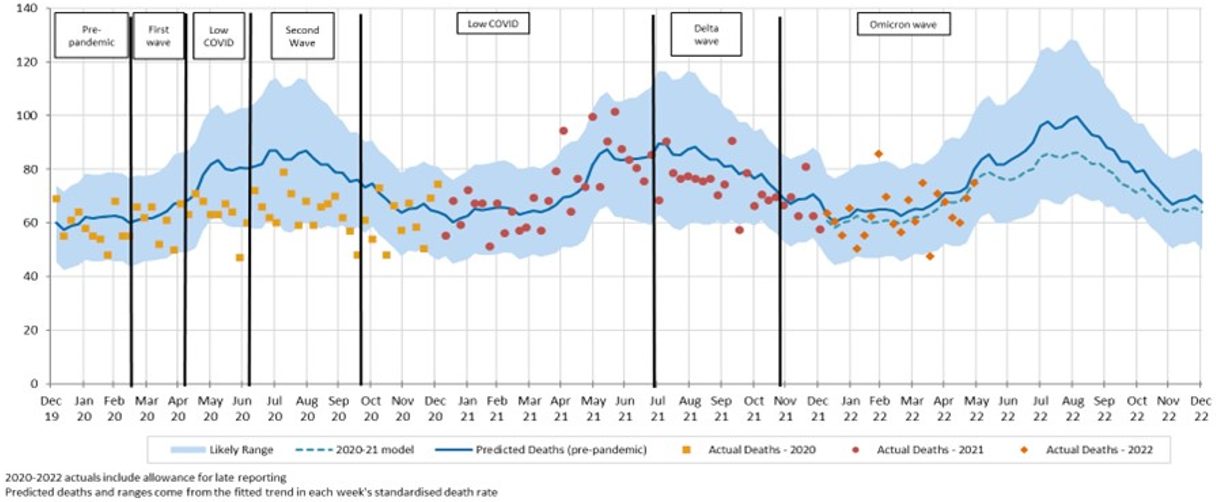
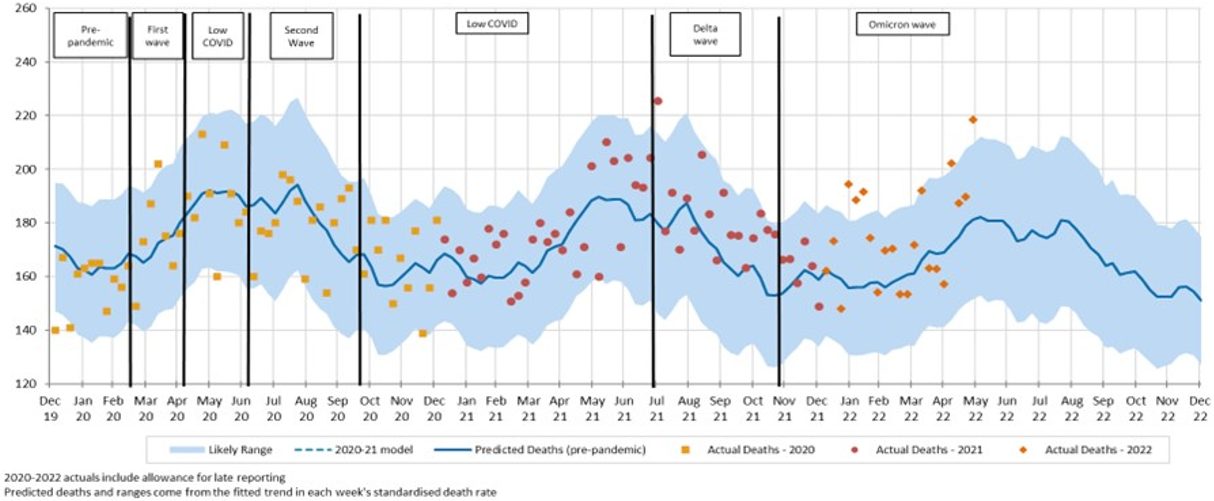
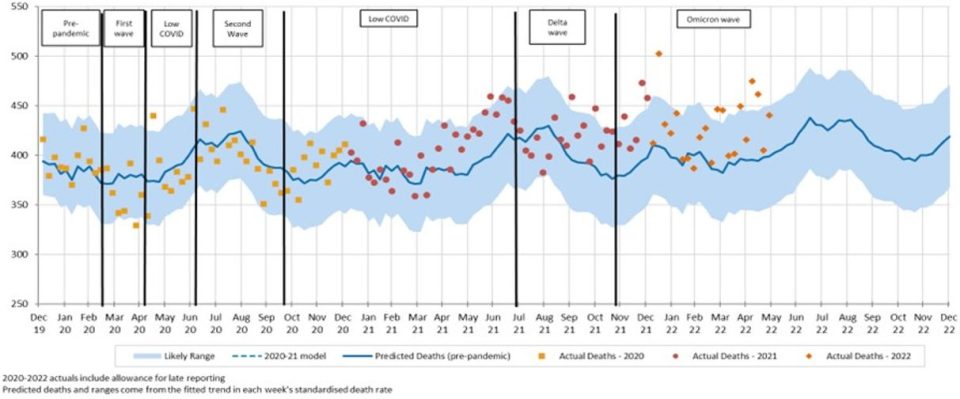
Figure 20 – Weekly actual and predicted coroner-referred deaths in Australia – All causes
Coroner-referred deaths continued to be higher than predicted every week in May 2022 and were above the prediction interval for the two of the five weeks of that month. Note that actual deaths data included in the graph includes coroner-referred deaths from COVID-19.
|
Members of the COVID-19 Mortality Working Group:
|
CPD: Actuaries Institute Members can claim two CPD points for every hour of reading articles on Actuaries Digital.