The implications of delays in cancer diagnosis
A concerning development associated with the COVID-19 pandemic has been that people have been unable to, or less inclined, to seek medical care and performing fewer diagnostic tests. Consequently, there will be both a delay in diagnosis and further progression of disease at diagnosis.
Left unaddressed, our health system would have to handle a higher frequency of treatment due to increased acuity, and each treatment would potentially be, on average, more complex, and (most likely) more expensive. Such a behavioural change to avoid or defer medical care, including diagnostic tests, would put upward pressure on total health costs and threaten a decline in health outcomes.
The focus of this article is the impact of delayed diagnostic procedures for colorectal cancer. However, we also present data that has generally shown fewer diagnostic tests and associated therapeutic procedures being performed during COVID-19. It is too early to tell if these trends are permanent or just a temporary effect of the pandemic and associated public health orders. With strong vaccination rates, it may be that these trends will start to revert to pre-COVID-19 levels of ‘normality’.
As actuaries, we have a role to try and make sense of this uncertainty, to help mitigate against this risk, and to understand and communicate the implications so that stakeholders can plan accordingly.
For the question at hand, uncertainty can be driven by behavioural changes:
- How has the rate of testing changed?
- How has the rate of seeking treatment changed, even after standardising for the stage of disease at diagnosis?
These behavioural changes interact with the natural progression of a disease that drives ultimate health outcomes. These, in turn, include:
- The rate of transition through different stages of the disease and the typical time spent at each stage
- A shift in the distribution of the stage of disease at point of detection
- The rate of survival by disease, by stage.
Actuaries can help piece these dynamics together using statistical modelling and collaborate with epidemiologists, clinicians, medical researchers and others to perform detailed analyses to help inform clinical pathways and implications for health system planning and funding.
Observed delays during COVID-19
In this section, we summarise recent observations around rates of diagnostic testing and therapeutic procedures. Cancer Australia recently published their report The Impact of COVID-19 on cancer-related medical services and procedures in Australia in 2020[1]. In summary, they analysed Medicare Benefits Schedule (MBS) claims data and observed that “when compared to the number of services expected, the sum of services examined across all cancer types observed nationally for 2020 for selected cancer-related diagnostic procedures was 8% lower than expected”.
A summary of observed versus expected ratios by cancer type is reproduced below from their report. ‘Expected’ is a Cancer Australia calculation based on an extrapolation of historical trends.
Table 1: Annual observed and expected services for cancer-related diagnostic procedures in 2020, by cancer type:
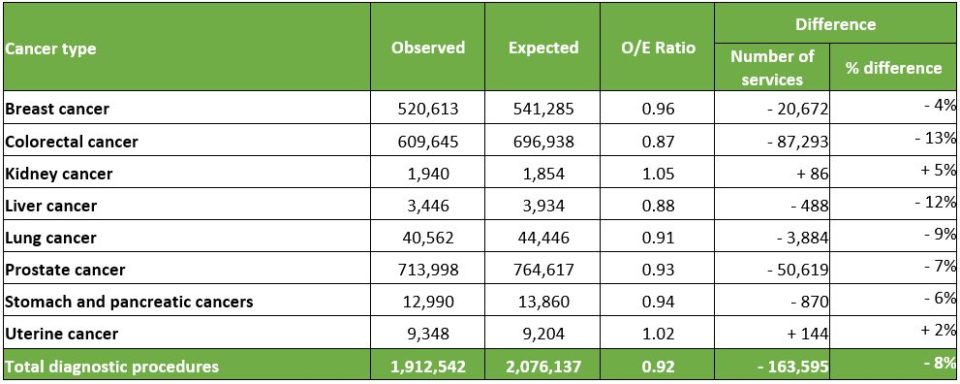
This data shows there has been a noticeable reduction in the rate of testing. However, this is not consistent across all forms of cancer with a higher observed than expected for kidney and uterine cancers.
From the same report, Cancer Australia also noted that “cancer-related surgical and non-surgical therapeutic procedures was 9% lower than expected” and provided the corresponding summary of observed versus expected ratios for treatment as reproduced below.
Table 2: Annual observed and expected services for cancer-related therapeutic procedures in 2020, by cancer type:
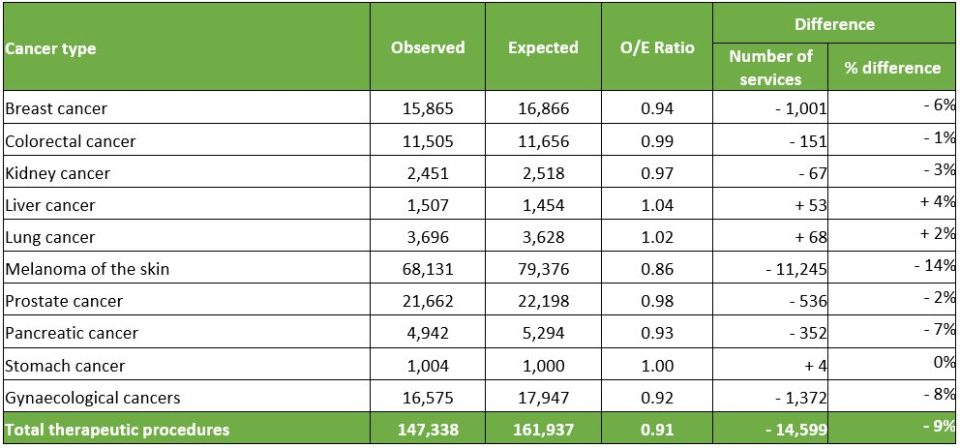
This data suggests that overall, there has also been a drop in the rate of therapeutic procedures. But again, we note that this has not been consistent across all forms of cancer with a higher observed than expected for liver and lung cancer.
However, for most cancers, it is hard to ignore the fact that lower-than-expected testing has coincided with lower-than-expected therapeutic procedures being performed. The below shows a scatterplot of the difference percentage for diagnostic (x-axis) versus therapeutic procedures (y-axis). We have added a diagonal line representing a scenario where the changes in the rate of diagnostic testing are ‘uniformly’ distributed across the stages of disease leading to a similar difference in the rate of therapeutic procedures being performed.
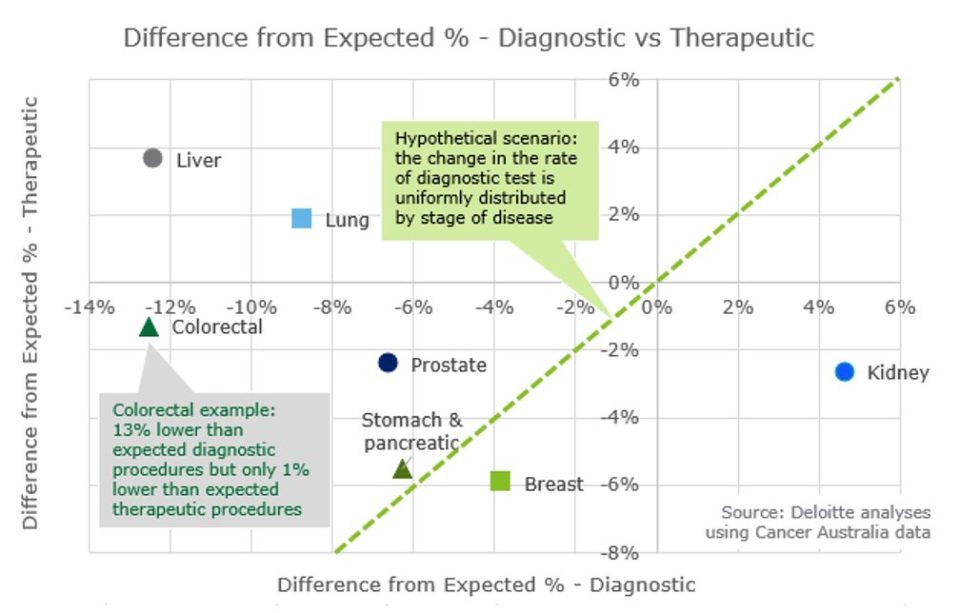
A key observation is that most of the observations are sitting in the bottom left quadrant where both diagnostic and therapeutic procedures are fewer than expected. However, this plot also shows that the change in diagnostic procedures does not always lead to a similar change in therapeutic procedures.
How can we interpret these observations?
- Behavioural impacts – perhaps relatively healthier people are not performing diagnostic procedures (e.g. prostate, colorectal)?
- Clinical impacts – in some cases, therapeutic procedures are actually higher than expected – could this already be a sign of increased progression of disease (e.g. liver, lung)?
- Clinical impacts – different cancers progress at different rates – how has their natural progression affected these observations? More latent and slower-growing cancers might see a delayed effect.
- Health system impacts – how much of the difference away from the diagonal line is just a result of increased waiting times for treatment due to system constraints?
It is not possible with this data to validate different hypotheses. However, it is clear that there are different ways to interpret it and that it would be useful to explore this uncertainty.
A modelling scenario – what is the impact of delayed diagnostic procedures for colorectal cancer?
To model the potential impact of a delay in diagnosis, we firstly calibrated our transition state model of disease progression to reflect the pre-COVID experience. We then altered the assumptions to reflect the delay in diagnosis to analyse the effect on utilisation and health outcomes.
The calibration involved ensuring that the model’s steady state distribution aligns with the observed distribution of stage of cancers. We have also relied on various medical research to derive some simplifying assumptions about the rate of transition. These were based on the typical time for a cancer to double in size amongst other factors.
Focusing on colorectal cancer, our scenario relies on the following simplifying assumptions that:
- diagnostic testing is uniformly distributed across the year;
- rate of seeking therapeutic treatment following a positive diagnosis for a given stage of cancer is not affected; and
- rate of survival for a given stage of cancer is not affected.
As would be expected, the model shows that the delay in diagnostic testing has a cascading impact on the distribution of cancer at each stage, producing a new COVID-19 impacted distribution. For colorectal cancer, the Cancer Australia data indicates that diagnostic procedures have been 13% lower than ‘expected’. This is equivalent to an average delay of diagnosis of 47 days leading our model to show that:
- the five-year survival rate decreases by 3.9% (meaning that for every 100 colorectal cancer patients, there will be almost four extra deaths within five years); and
- a 23% increase in the number of Stage 4 cancers implying a significant increase in the utilisation rate of cancer treatments for this stage of cancer.
The implications of this scenario are far reaching. Aside from the direct effects on hospital utilisation, and health and mortality outcomes, there are also implications for critical illness claims as the delays in diagnoses leads to an increase in progression to more advanced stages of cancer. If more people are seeking treatment at more advanced stages of cancer, there are potentially mental health pressures from more prolonged treatment. This may create additional insurance claims for mental health, whether it be in private health insurance or income protection or others.
With more data, further insights could be derived from this scenario. For example, having treatment costs at different stages of cancer could inform the overall funding implications for our health system. The upstream impact from changes in participation of publicly run and complementary cancer screening programs would add an extra observation to understand their downstream effect on utilisation of diagnostic or therapeutic procedures.
Ultimately, this is a scenario only, based on a number of simplifying assumptions and these results should be considered in that context. In the real world, the delay in diagnostic testing may just be a temporary phenomenon, rather than a permanent shift as this scenario is constructed. One could argue this scenario is conservative in the sense that it is overstating the delay in procedures and represents an adverse shift in the distribution of stages of cancer.
This type of actuarial modelling can bring insights into helping the health system understand the nature of this uncertainty with implications for various types of insurance. We can collaborate with other health professionals to explore how scenarios might play out and bring our particular angle to the problem.
|
[1] – Cancer Australia. The impact of COVID-19 on cancer-related medical services and procedures in Australia in 2020: Examination of MBS claims data for 2020, nationally and by jurisdiction. 2021; Available from: https://www.canceraustralia.gov.au/the-impact-of-COVID-19-on-cancer-related-medical-services-and-procedures-in-Australia-in-2020.
|
CPD: Actuaries Institute Members can claim two CPD points for every hour of reading articles on Actuaries Digital.